Psychedelics in the Treatment of Unipolar Mood Disorders a Systematic Review
Results
We included 83 published reports in this systematic review (see Fig. ane for PRISMA flow diagram), comprising 33 systematic reviews (of which 17 included meta-analyses), 29 RCTs, two randomised trials with no placebo control, three non-randomised trials with controls, half-dozen open up-label trials and ten retrospective reviews. A list of studies that appeared to come across the inclusion criteria only were excluded, and reasons for exclusions, are provided in Supplementary Table ane.
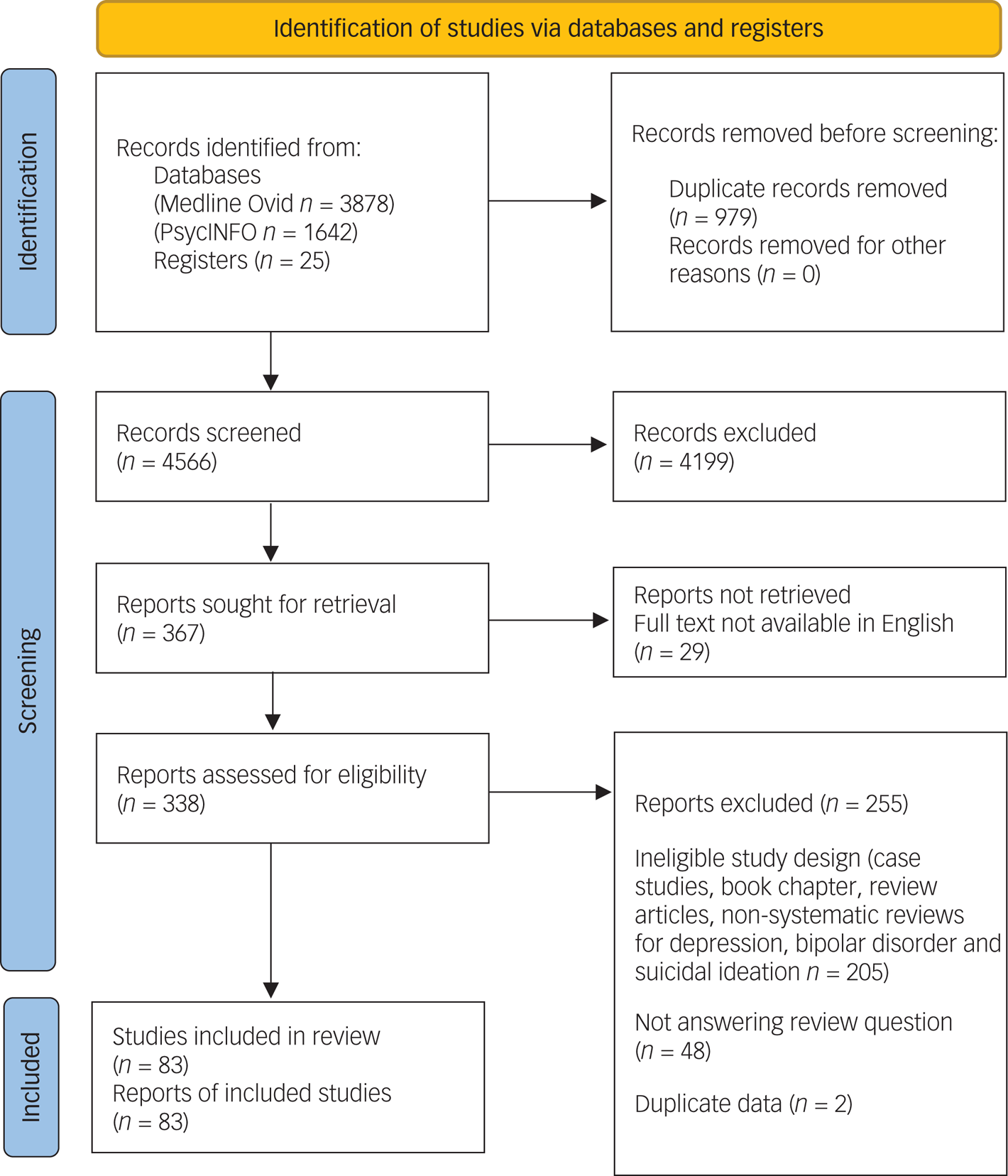
Fig. one Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 menstruum diagram for new systematic reviews that included searches of databases and registers but. Diagram template obtained from Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71.
Unipolar depression and MDD
We identified 24 systematic reviews of the antidepressant effect of ketamine in the treatment of unipolar depression and/or MDD, 12 of which conducted meta-analyses. In general, reviews consistently identified a robust, rapid, and typically curt-lived antidepressant consequence for ketamine.
All systematic review or meta-analytic manufactures noted rapid onset of ketamine's antidepressant effect among patients with MDD. Reference Aan Het Rot, Zarate, Charney and Mathewthree,Reference Serafini, Howland, Rovedi, Girardi and Amore4,Reference Fond, Loundou, Rabu, Macgregor, Lançon and Brittnersix–Reference Lee, Della Selva, Liu and Himelhochix,Reference Romeo, Choucha, Fossati and Rotge14,Reference Katalinic, Lai, Somogyi, Mitchell, Glue and Loo15,Reference Caddy, Giaroli, White, Shergill and Tracyforty–Reference Papakostas, Salloum, Hock, Jha, Murrough and Mathew53 Meta-analyses, which primarily focused on a single intravenous infusions, identified lower mean depression severity and remission in ketamine groups relative to placebo, with onset between 1 and 24 h post-infusion, Reference Fond, Loundou, Rabu, Macgregor, Lançon and Brittner6,Reference Lee, Della Selva, Liu and Himelhochix,Reference Romeo, Choucha, Fossati and Rotgefourteen,Reference Caddy, Giaroli, White, Shergill and Tracy40,Reference Caddy, Amit, McCloud, Rendell, Furukawa and McShane41,Reference Coyle and Laws43,Reference Han, Chen, Zou, Zheng, Li and Wang45,Reference Kishimoto, Chawla, Hagi, Zarate, Kane and Bauer47,Reference McGirr, Berlim, Bail, Fleck, Yatham and Lamfifty,Reference Zheng, Cai, Xiang, Zheng, Jiang and Sim52 and typically persisting for 1–ii weeks. Reference Aan Het Rot, Zarate, Charney and Mathew3,Reference Kraus, Rabl, Vanicek, Carlberg, Popovic and Spies8,Reference Lee, Della Selva, Liu and Himelhoch9,Reference Romeo, Choucha, Fossati and Rotgefourteen,Reference Caddy, Amit, McCloud, Rendell, Furukawa and McShane41–Reference Coyle and Laws43,Reference Han, Chen, Zou, Zheng, Li and Wang45,Reference Kishimoto, Chawla, Hagi, Zarate, Kane and Bauer47,Reference Kolar49,Reference McGirr, Berlim, Bond, Flake, Yatham and Laml Repeated administrations of ketamine of up to six doses produce a more than pronounced antidepressant effect at the 2-calendar week follow-upward relative to a unmarried administration, Reference Coyle and Laws43,Reference Garay, Zarate, Charpeaud, Citrome, Correll and Hameg44,Reference McGirr, Berlim, Bond, Fleck, Yatham and Lam50 and prolonged fourth dimension to relapse. Reference Aan Het Rot, Zarate, Charney and Mathewiii,Reference Katalinic, Lai, Somogyi, Mitchell, Glue and Looxv,Reference Garay, Zarate, Charpeaud, Citrome, Correll and Hameg44,Reference Kishimoto, Chawla, Hagi, Zarate, Kane and Bauer47,Reference McGirr, Berlim, Bail, Fleck, Yatham and Lam50
Studies on routes of administration other than intravenous betoken an antidepressant event comparable with that of intravenous assistants. Reference Serafini, Howland, Rovedi, Girardi and Affection4,Reference Lee, Della Selva, Liu and Himelhoch9,Reference Romeo, Choucha, Fossati and Rotge14,Reference Garay, Zarate, Charpeaud, Citrome, Correll and Hameg44,Reference Jankauskas, Necyk, Chue and Chue46,Reference Zheng, Cai, Xiang, Zheng, Jiang and Sim52 One meta-assay demonstrated that adjunctive intranasal ketamine was significantly more effective than placebo for reducing depressive symptoms, response and remission from depression. Reference Papakostas, Salloum, Hock, Jha, Murrough and Mathew53 A direct comparison of intravenous versus intramuscular ketamine for depression concluded that the methods were equivalent in terms of safety and effectiveness. Reference Chilukuri, Reddy, Pathapati, Manu, Jollu and Shaik13 With regards to oral ketamine, a systematic review reported that repeated administration of oral ketamine was well-tolerated and had medium-to-large effect sizes, with a delay of 2–6 weeks before the emergence of clinically significant antidepressant furnishings. Reference Rosenblat, Carvalho, Li, Lee, Subramanieapillai and McIntyre54 A meta-assay comparison intravenous, intranasal and oral ketamine administrations was inconclusive because of heterogeneity across studies, simply noted that furnishings for intravenous ketamine appeared to peak at 2–6 days, compared with 24 h for intranasal administration and vii–twenty days for oral administration, potentially because of increasing bioavailability over fourth dimension. Reference McIntyre, Carvalho, Lui, Majeed, Masand and Gill55
Ketamine is effective both in trials restricted to patients with treatment-resistant low (i.e. non-response to prior antidepressant trials) and trials that included patients who had responded to prior handling. Reference Fond, Loundou, Rabu, Macgregor, Lançon and Brittner6,Reference Han, Chen, Zou, Zheng, Li and Wang45 Likewise, ketamine's effect has been identified in patients who are currently taking other antidepressant medications, as well every bit those who are drug-free or have completed a washout menses. Reference Fond, Loundou, Rabu, Macgregor, Lançon and Brittner6,Reference Caddy, Amit, McCloud, Rendell, Furukawa and McShane41,Reference Jankauskas, Necyk, Chue and Chue46,Reference Kolar49
Bipolar disorder
The majority of enquiry on ketamine treatment for bipolar disorder has involved adults identified as resistant to prior handling, and primarily tested ketamine as an offshoot to other treatments such equally mood stabilisers or ECT. Reference Katalinic, Lai, Somogyi, Mitchell, Glue and Loo15,Reference Alberich, Martínez-Cengotitabengoa, López, Zorrilla, Núñez and Vieta56 Nosotros identified 17 systematic reviews of the antidepressant effect of ketamine in the treatment of bipolar disorder, 9 of which included meta-analyses. I review Reference Alberich, Martínez-Cengotitabengoa, López, Zorrilla, Núñez and Vieta56 and ii meta-analyses Reference McCloud, Caddy, Jochim, Rendell, Diamond and Shuttleworth57,Reference Fornaro, Carvalho, Fusco, Anastasia, Solmi and Berk58 focused exclusively on bipolar disorder, whereas the remaining 14 likewise reviewed unipolar depression.
Similar to unipolar depression, the reviews found a rapid and short-lived antidepressant effects of ketamine in patients with bipolar disorder. Reference Fond, Loundou, Rabu, Macgregor, Lançon and Brittner6,Reference Kraus, Rabl, Vanicek, Carlberg, Popovic and Spiesviii,Reference Lee, Della Selva, Liu and Himelhoch9,Reference Romeo, Choucha, Fossati and Rotge14,Reference McGirr, Berlim, Bond, Scrap, Yatham and Laml,Reference Alberich, Martínez-Cengotitabengoa, López, Zorrilla, Núñez and Vieta56,Reference McCloud, Caddy, Jochim, Rendell, Diamond and Shuttleworth57 Meta-analyses identified effects with onset as early as 4 h Reference Coyle and Laws43 and consistently by 24 h. Reference Fond, Loundou, Rabu, Macgregor, Lançon and Brittner6,Reference Lee, Della Selva, Liu and Himelhochix,Reference Romeo, Choucha, Fossati and Rotgexiv,Reference McGirr, Berlim, Bond, Fleck, Yatham and Lam50,Reference McCloud, Caddy, Jochim, Rendell, Diamond and Shuttleworth57,Reference Fornaro, Carvalho, Fusco, Anastasia, Solmi and Berk58 Findings are less consequent with respect to duration, with some analyses concluding that furnishings are limited to 3 days Reference Romeo, Choucha, Fossati and Rotge14,Reference McCloud, Caddy, Jochim, Rendell, Diamond and Shuttleworth57 and others reporting that effects retain superiority over placebo at vii days. Reference Coyle and Laws43,Reference McGirr, Berlim, Bail, Chip, Yatham and Laml Meta-analyses at 14 days did not detect an effect of ketamine. Reference Romeo, Choucha, Fossati and Rotgefourteen,Reference Coyle and Laws43,Reference McCloud, Caddy, Jochim, Rendell, Diamond and Shuttleworth57,Reference Fornaro, Carvalho, Fusco, Anastasia, Solmi and Berk58
Comparisons of effect size in unipolar versus bipolar depression populations have non yielded consistent results. A meta-analysis plant no difference at four h after administration, and ii out of three meta-analyses reported no difference at 24 h afterward infusion; in contrast, one meta-assay found a larger antidepressant outcome for MDD at 24 h. Reference Lee, Della Selva, Liu and Himelhoch9,Reference Coyle and Laws43,Reference McGirr, Berlim, Bond, Flake, Yatham and Lam50 Similarly, equivocal results are seen at seven-day follow-up: one meta-assay identified a stronger effect in bipolar low Reference Coyle and Laws43 and ane found no difference. Reference McGirr, Berlim, Bond, Chip, Yatham and Lamfifty Notably, the vii meta-analyses included in the present review rely on information extracted from ii RCTs conducted past the aforementioned enquiry group. Reference Diazgranados, Ibrahim, Brutsche, Newberg, Kronstein and Khalife59,Reference Zarate, Brutsche, Ibrahim, Franco-Chaves, Diazgranados and Cravchik60 In sum, extant findings do not support a consequent difference in ketamine effects on depressive episodes in MDD versus bipolar disorder.
The main business concern of ketamine treatment for bipolar disorder is the hazard of inducing mania. Although manic symptoms in patients with bipolar disorder accept been noted to increase immediately following ketamine infusion, these symptoms tend to resolve within 1 or 2 h. Reference Fond, Loundou, Rabu, Macgregor, Lançon and Brittner6,Reference Romeo, Choucha, Fossati and Rotge14,Reference Alberich, Martínez-Cengotitabengoa, López, Zorrilla, Núñez and Vieta56 In a meta-analysis, information technology was reported that treatment emergent mania was not observed statistically significantly more oftentimes in the active intervention group compared with the placebo. Reference Fornaro, Carvalho, Fusco, Anastasia, Solmi and Berk58 Even so, this meta-analysis is probably underpowered to detect uncommon adverse furnishings such every bit mania. Reference Fornaro, Carvalho, Fusco, Anastasia, Solmi and Berk58–Reference Zarate, Brutsche, Ibrahim, Franco-Chaves, Diazgranados and Cravchikthreescore
Likewise, prove from instance studies, open-label trials and retrospective chart analyses suggest that non-intravenously (i.e. intramuscular, intranasal and oral) administered ketamine is effective and safe for adults with bipolar disorder. Reference Aan Het Rot, Zarate, Charney and Mathewthree,Reference Dore, Turnipseed, Dwyer, Turnipseed, Andries and Ascani12,Reference Katalinic, Lai, Somogyi, Mitchell, Mucilage and Loo15,Reference Rosenblat, Carvalho, Li, Lee, Subramanieapillai and McIntyre54,Reference Alberich, Martínez-Cengotitabengoa, López, Zorrilla, Núñez and Vieta56
Suicidal ideation
We identified vi systematic reviews of the effects of ketamine on suicidal ideation, Reference Reinstatler and Youssef61–Reference Witt, Potts, Hubers, Grunebaum, Murrough and Loo66 ii of which included a meta-analysis of studies Reference Bartoli, Riboldi, Crocamo, Di Brita, Clerici and Carrà62,Reference Witt, Potts, Hubers, Grunebaum, Murrough and Loo66 and one with a meta-analysis of individual participant data. Reference Wilkinson, Ballard, Bloch, Mathew, Murrough and Feder63 The ketamine doses ranged from 0.ane to three mg/kg, and were virtually ofttimes administered intravenously, although oral intermission, intranasal, intramuscular and subcutaneous bolus infusions have also been used in a number of studies. Reference Reinstatler and Youssef61,Reference Bartoli, Riboldi, Crocamo, Di Brita, Clerici and Carrà62,Reference D'Anci, Uhl, Giradi and Martin64–Reference Witt, Potts, Hubers, Grunebaum, Murrough and Loo66 Ii reviews were limited to trials of a single dose of ketamine, Reference Bartoli, Riboldi, Crocamo, Di Brita, Clerici and Carrà62,Reference Wilkinson, Ballard, Bloch, Mathew, Murrough and Feder63 and the other reviews included studies of multiple doses of ketamine, only did not straight compare doses. Reference Reinstatler and Youssef61,Reference D'Anci, Uhl, Giradi and Martin64–Reference Witt, Potts, Hubers, Grunebaum, Murrough and Loo66 Further information comparison the condom and efficacy of single and repeated doses of ketamine for suicidal ideation is needed.
The one review that examined road of assistants found no differences between a bolus dose (0.2 mg/kg) and an infusion (0.5 mg/kg). Reference Bartoli, Riboldi, Crocamo, Di Brita, Clerici and Carrà62 Nonetheless, in that location is express testify on intramuscular, intranasal and oral formulations for use in suicidal ideation. Reference Dadiomov and Lee65 Additionally, in one study of intranasal esketamine, no participants managed to self-administer the ten pumps to receive the full dose, because of adverse effects; suggesting that the tolerability of intranasal administration may exist poor. Reference Witt, Potts, Hubers, Grunebaum, Murrough and Loo66,Reference Gálvez, Li, Huggins, Glue, Martin and Somogyi67
All meta-analyses and systematic reviews concluded that ketamine handling was associated with a moderate-to-big decrease in suicidal ideation (Cohen's d = 0.51–0.85). Reference Reinstatler and Youssef61–Reference Witt, Potts, Hubers, Grunebaum, Murrough and Loo66 These furnishings appeared within the beginning 4 h of treatment Reference Reinstatler and Youssef61,Reference Bartoli, Riboldi, Crocamo, Di Brita, Clerici and Carrà62,Reference Witt, Potts, Hubers, Grunebaum, Murrough and Loo66 and were maintained for an average of 3 days Reference Reinstatler and Youssef61,Reference Witt, Potts, Hubers, Grunebaum, Murrough and Loo66 up to a calendar week, Reference Wilkinson, Ballard, Bloch, Mathew, Murrough and Feder63,Reference Dadiomov and Lee65 although long-term effects are not reported. Reference Dadiomov and Lee65 Among participants who showed remission of suicidal ideation within 24 h of handling, the treatment result persisted for upwardly to 1 week in approximately 85% of participants. Interestingly, ketamine effects remained pregnant subsequently adjusting for alter in low, suggesting that ketamine may accept anti-suicidal furnishings independent of antidepressant effects. Reference Wilkinson, Ballard, Bloch, Mathew, Murrough and Feder63,Reference Dadiomov and Lee65 In one meta-assay, one of the studies included data on suicide attempts upwards to 28 days after treatment; no participants had attempted suicide in either the ketamine or placebo group during this time period. Reference Witt, Potts, Hubers, Grunebaum, Murrough and Loo66 Interestingly, in some other review it was reported that ketamine led to transient improvements in suicidal ideation in individuals who had been admitted to hospital because of a suicide attempt or in those with chronic and astringent suicidal ideation. Reference Dadiomov and Lee65 Although these data were based on case reports, this high suicide hazard population has been excluded from other trials. Reference Dadiomov and Lee65
Interactions with ECT
The combined anaesthetic and antidepressant action of ketamine make it a logical choice for use in ECT, with the hope that it might exert additive or perhaps synergistic effects. Reference Kellner and Iosifescu68 We identified 19 studies of patients with MDD, bipolar disorder and treatment-resistant depression, in which ketamine was either used as an anaesthetic during ECT or for relapse prevention following ECT treatment. All studies used intravenous administration with doses ranging from 0.5 to two mg/kg. Ketamine was superior in reducing depressive symptoms in 8 of the xviii studies when compared with an active control such every bit methohexital, thiopental or propofol. Reference Gamble, Bi, Bowen, Weisgerber, Sanjanwala and Prasad69–Reference Salehi, Mohammadbeigi, Kamali, Taheri-Nejad and Moshiri82
The most consistent evidence for event of ketamine with ECT is in the treatment of treatment-resistant depression: three double-blind RCTs, one partially randomised trial, one open-label trial and 1 retrospective review take reported positive findings for the impact of ketamine on the effectiveness of ECT for treatment-resistant depression, whereas three RCTs reported no differences between ketamine and placebo. Reference Zhang, Rosenheck, Lin, Li, Zhou and Xiao83,Reference Altinay, Karne and Anand84 In general, these studies reported that, relative to other anaesthetics, ketamine was associated with before improvements in depression, college remission rate, better overall comeback longer seizure duration, fewer required ECT sessions and less cognitive impairment (but see likewise Carspecken et al Reference Carspecken, Borisovskaya, Lan, Heller, Buchholz and Ruskin79). Reference Gamble, Bi, Bowen, Weisgerber, Sanjanwala and Prasad69–Reference Okamoto, Nakai, Sakamoto, Nagafusa, Higuchi and Nishikawa71,Reference Rybakowski, Bodnar, Krzywotulski, Chlopocka-Wozniak, Michalak and Rosada-Kurasinska76,Reference Zhong, He, Zhang, Wang, Jiang and Li78,Reference Salehi, Mohammadbeigi, Kamali, Taheri-Nejad and Moshiri82
In contrast to findings demonstrating the benefit of ketamine every bit an adjunct to ECT for treatment-resistant depression, results from MDD and bipolar disorder are less supportive. A double-blind RCT of 31 in-patients with MDD reported a more than rapid antidepressant effect, lower required electric dose and longer seizure duration with ketamine amazement during ECT. Reference Yoosefi, Sepehri, Kargar, Akhondzadeh, Sadeghi and Rafei77 In a larger RCT with 172 patients, low-dose (0.3 mg/kg) ketamine-assisted ECT was associated with college remission rate compared with routine ECT with propofol; interestingly, intermittent ketamine administration (one in every three ECT sessions) resulted in lower rates of psychiatric complications compared with repeated ketamine administration with each ECT session. Reference Dong, Min, Qiu, Chen and Ren85
Nonetheless, results from half dozen other studies propose no departure between ECT with ketamine and ECT with control atmospheric condition in reducing depressive symptoms in those with MDD or bipolar disorder, Reference Anderson, Blamire, Branton, Brigadoi, Clark and Downey73–Reference Shams-Alizadeh, Maroufi, Nasseri, Najafabadi, Taghiabad and Gharibi75,Reference Fernie, Currie, Perrin, Stewart, Anderson and Bennettfourscore,Reference Rasmussen, Kung, Lapid, Oesterle, Geske and Nuttall81,Reference Ray-Griffith, Eads, Han, Golden and Stowe86 although one study was reported to lack power because of small sample size. Reference Ray-Griffith, Eads, Han, Golden and Stowe86 Divergent results may be a result of differences in effectiveness for adjunctive ketamine in ECT, simply may as well reverberate differences in handling equally the optimal dosage and frequency remains undetermined. Indeed, studies that reported no do good for ketamine mostly involved lower doses of 0.3–0.5 mg/kg, Reference Anderson, Blamire, Branton, Brigadoi, Clark and Downey73–Reference Shams-Alizadeh, Maroufi, Nasseri, Najafabadi, Taghiabad and Gharibi75 just non always. Reference Ray-Griffith, Eads, Han, Gilded and Stowe86
Aside from the use of ketamine as an anaesthetic agent during ECT, 1 airplane pilot study aimed to examine the effectiveness of ketamine for relapse prevention following response to ECT. Reference Finnegan, Galligan, Ryan, Shanahan, Harkin and Daly87 However, out of 26 patients who responded to ECT treatment, simply six were willing to take function, some because of a lack of interest in further treatment following successful ECT, and none of the participants completed the full iv-week treatment protocol. Reference Finnegan, Galligan, Ryan, Shanahan, Harkin and Daly87
Social feet and generalised anxiety disorder
We identified 6 studies of ketamine treatment for social anxiety disorder and/or generalised anxiety disorder (GAD). A retrospective review of patients receiving multiple sessions of ketamine assisted therapy (sublingual and/or intramuscular) in a private practise setting, revealed meaning subtract in anxiety following treatment compared with baseline. Reference Dore, Turnipseed, Dwyer, Turnipseed, Andries and Ascani12 A report of open-label ascending dose ketamine (0.25, 0.5 and 1 mg/kg intramuscular at 7-day intervals) among 12 patients with treatment refractory social anxiety disorder and/or generalised anxiety disorder reported that 1 mg/kg was associated with the greatest duration of anxiolytic effects for up to vii days after infusion. Reference Glue, Medlicott, Harland, Neehoff, Anderson-Fahey and Le Nedelec34 Following the 0.5 mg/kg or i mg/kg doses, ten out of 12 patients reported a 50% or more reduction in anxiety and/or fearfulness. Reference Glue, Medlicott, Harland, Neehoff, Anderson-Fahey and Le Nedelec34 In a double-bullheaded study, 12 patients with treatment-resistant generalised anxiety disorder and/or social anxiety disorder received three ascending doses of ketamine (0.25, 0.5 and one mg/kg) and midazolam (0.01 mg/kg) at 1-calendar week intervals. Reference Shadli, Kawe, Martin, McNaughton, Neehoff and Gum88 Viii out of the 12 patients experienced at to the lowest degree a 50% reduction in anxiety and/or fearfulness. Reference Shadli, Kawe, Martin, McNaughton, Neehoff and Glue88 A subsequent study from the same investigators reported dose-related decreases in scores on measures of feet and fright. Reference Glue, Neehoff, Sabadel, Broughton, Le Nedelec and Shadli89 These studies Reference Gum, Medlicott, Harland, Neehoff, Anderson-Fahey and Le Nedelec34,Reference Shadli, Kawe, Martin, McNaughton, Neehoff and Glue88,Reference Glue, Neehoff, Sabadel, Broughton, Le Nedelec and Shadli89 established a higher dose of ketamine (1 mg/kg) equally having the greatest and most durable anxiolytic effects, although ane reported dose-related improvements in fearfulness, just non anxiety symptoms. Reference Shadli, Kawe, Martin, McNaughton, Neehoff and Glue88
Participants who responded to ketamine handling in the previous two studies Reference Glue, Medlicott, Harland, Neehoff, Anderson-Fahey and Le Nedelec34,Reference Gum, Neehoff, Sabadel, Broughton, Le Nedelec and Shadli89 were enrolled in an open-label maintenance treatment study for 14 weeks (north = 20), where they received repeated doses of 1 mg/kg of ketamine over 12 weeks, with the dose frequency adjusted co-ordinate to the elapsing of response to ketamine. Reference Glue, Neehoff, Medlicott, Gray, Kibby and McNaughton35 Patients who responded to initial ketamine treatment remained in remission with maintenance treatment over iii months; however, the recurrence of symptoms was common within 2 weeks of stopping treatment. Reference Gum, Neehoff, Medlicott, Gray, Kibby and McNaughton35
A cantankerous-over RCT of a single dose of ketamine (0.five mg/kg) for social anxiety disorder reported that ketamine led to significantly greater number of responders compared with placebo, with half-dozen out of 18 participants experiencing a reduction in clinician-rated anxiety scores of at least 35%, compared with none of 17 participants who received placebo. Reference Taylor, Landeros-Weisenberger, Coughlin, Mulqueen, Johnson and Gabriel90 Similarly, 16 out of 18 participants who received ketamine experienced 50% or more reduction in self-reported anxiety scores, compared with nine out of 17 in the placebo group; this group difference was statistically pregnant. Reference Taylor, Landeros-Weisenberger, Coughlin, Mulqueen, Johnson and Gabriel90
Obsessive–compulsive disorders
Nosotros identified two studies. First, in a cross-over RCT, patients without depression and with chronic and treatment-resistant obsessive–compulsive disorder who received a unmarried dose of intravenous ketamine had lower obsessive–compulsive disorder scores than those receiving placebo at 4 h and at vii days following the infusion. Reference Rodriguez, Kegeles, Levinson, Feng, Marcus and Vermes91 Half of those receiving ketamine demonstrated a 35% or more than reduction in obsessive–compulsive disorder symptoms, compared with none of the placebo group. An open-label trial of a single dose of ketamine (0.v mg/kg intravenous) in 10 participants with severe treatment refractory obsessive–compulsive disorder found a significant just transient do good in clinician-rated obsessive–compulsive disorder symptoms at i–3 h later infusion. Reference Bloch, Wasylink, Landeros-Weisenberger, Panza, Billingslea and Leckman92
Postal service-traumatic stress disorder
Eight publications that investigated the association betwixt ketamine and post-traumatic stress disorder were identified. Ane RCT Reference Feder, Parides, Murrough, Perez, Morgan and Saxena93 and two open up-label trials expressly focused on ketamine treatment for postal service-traumatic stress disorder symptoms, Reference Albott, Lim, Forbes, Erbes, Tye and Grabowski94,Reference Ross, Jain, Bonnett and Wolfson95 whereas the other v retrospectively examined the effects of peri-traumatic anaesthetic ketamine administration during treatment for physical injury. Reference Schönenberg, Reichwald, Domes, Badke and Hautzinger96–Reference Highland, Soumoff, Spinks, Kemezis and Buckenmaier100
The first retrospective study found that patients who were administered ketamine following trauma exposure demonstrated increased post-traumatic stress disorder symptoms at 1 yr, Reference Schönenberg, Reichwald, Domes, Badke and Hautzinger96 and a subsequent study by the same grouping identified increased symptoms of acute stress disorder, a precursor to post-traumatic stress disorder, iii days subsequent to emergency treatment in people given ketamine compared with opioid and other analgesics. Reference Schönenberg, Reichwald, Domes, Badke and Hautzinger97
Iii studies examining mail-traumatic stress disorder in USA military machine personnel who had been administered ketamine for service-related injuries reported conflicting results. In the beginning study, receiving perioperative ketamine was associated with lower mail-traumatic stress disorder prevalence (27% compared with 46%) among those who had not received ketamine, despite increased burn size, longer hospital stay and increased number of operations in the ketamine group. Reference McGhee, Maani, Garza, Gaylord and Blackness98 Ketamine use during surgical procedures as well had a significant only weak negative correlation with postal service-traumatic stress disorder. Reference McGhee, Maani, Garza, Gaylord and Blackness98 In contrast, two subsequent studies reported comparable rates of mail-traumatic stress disorder and postal service-traumatic stress disorder symptoms among ketamine and non-ketamine groups, although one of these studies was reported to have low power (<%80). Reference McGhee, Maani, Garza, Slater, Petz and Fowler99,Reference Highland, Soumoff, Spinks, Kemezis and Buckenmaier100
Iii studies focused on ketamine for the treatment of post-traumatic stress disorder. An open-label trial of vi infusions (0.v mg/kg) over 12 days in 15 military veterans with chronic postal service-traumatic stress disorder and depression reported a pregnant subtract in mail-traumatic stress disorder and low symptoms 24 h afterwards the terminal infusion. Reference Albott, Lim, Forbes, Erbes, Tye and Grabowski94 At 14 days mail-treatment, 80% of the sample were in remission from mail-traumatic stress disorder symptoms, and forty% remained in remission at the end of the 56-solar day follow-up period. Reference Albott, Lim, Forbes, Erbes, Tye and Grabowski94 Similarly, in another open-label report, 30 participants received half dozen ketamine infusions commencement at 1 mg/kg; a significant reduction (44%) in postal service-traumatic stress disorder symptoms was observed from baseline to earlier the sixth infusion. Reference Ross, Jain, Bonnett and Wolfson95 A cross-over RCT of a single intravenous subanaesthetic dose of ketamine (0.5 mg/kg) amid 41 patients with chronic post-traumatic stress disorder reported that post-traumatic stress disorder symptom severity was improved compared with midazolam at 24 h, merely not at 7 days. Reference Feder, Parides, Murrough, Perez, Morgan and Saxena93
Substance apply disorders
We identified 14 studies examining ketamine as a treatment for substance use disorders, including 6 studies focusing on booze utilize disorder, Reference Krupitsky, Grineko, Berkaliev, Paley, Tetrov and Mushkov16,Reference Krupitsky and Grinenko17,Reference Wong, Bridegroom, Armahizer and Kane-Gill101–Reference Dakwar, Levin, Hart, Basaraba, Choi and Pavlicova104 five on cocaine use disorder Reference Dakwar, Nunes, Hart, Hu, Foltin and Levin31,Reference Dakwar, Anerella, Hart, Levin, Mathew and Nunes105–Reference Dakwar, Nunes, Hart, Foltin, Mathew and Carpenter108 and three on opiate utilize disorder. Reference Krupitsky, Burakov, Romanova, Dunaevsky, Strassman and Grinenkoeighteen,Reference Krupitsky, Burakov, Dunaevsky, Romanova, Slavina and Grinenko19,Reference Jovaiša, Laurinėnas, Vosylius, Šipylaitė, Badaras and Ivaškevičius109
Alcohol use disorders
One study examined ketamine in combination with aversive therapy approaches that aim to found negative links between alcohol consumption and booze's detrimental effect. Reference Krupitsky, Grineko, Berkaliev, Paley, Tetrov and Mushkovxvi It was reported that seventy% of participants in the ketamine group remained abstinent at 1 year compared with 24% of participants who received aversion therapy alone. Reference Krupitsky, Grineko, Berkaliev, Paley, Tetrov and Mushkovsixteen A subsequent study compared in-patients who selected KAP versus conventional psychotherapy reported 12-month abstinence rates of 66% for the ketamine group compared with 24% of controls. Reference Krupitsky and Grinenko17
More than xx years afterwards, an RCT of a single ketamine intravenous infusion (0.71 mg/kg) paired with motivational enhancement therapy for alcohol dependence reported that ketamine significantly increased abstinence rates and led to a lower likelihood of alcohol use and heavy drinking, and longer time to relapse over 21 days afterwards infusion, compared with midazolam. Reference Dakwar, Levin, Hart, Basaraba, Choi and Pavlicova104 Of those available at 6-month follow-up, 75% in the ketamine group reported abstinence, whereas simply 27% did so in the midazolam grouping. Reference Dakwar, Levin, Hart, Basaraba, Choi and Pavlicova104
Ketamine may besides have a role in the detoxification stage of treatment: iii retrospective cohort studies of the safety and efficacy of ketamine for the management of alcohol withdrawal syndrome ended that ketamine was safe. Reference Wong, Benedict, Armahizer and Kane-Gill101–Reference Pizon, Lynch, Benedict, Yanta, Frisch and Menke103
Cocaine use disorders
Three studies by a single inquiry grouping have investigated ketamine administration on individuals with cocaine use disorders. An experimental written report in cocaine dependent volunteers reported that a single dose of ketamine (0.41 mg/kg) increased motivation to quit cocaine and reduced cue induced craving significantly more than lorazepam at 24-h follow-upwards. Reference Dakwar, Levin, Foltin, Nunes and Hart106 The 2nd dose (0.71 mg/kg) further decreased cue-induced peckish for an boosted twenty-four hours subsequently administration. Reference Dakwar, Levin, Foltin, Nunes and Hart106 At 4 weeks, all participants reported a significant reduction in amount and frequency of cocaine use. Reference Dakwar, Levin, Foltin, Nunes and Hart106 A 2nd report on the aforementioned participants indicated that these effects were mediated by ketamine-induced mystical experiences. Reference Dakwar, Anerella, Hart, Levin, Mathew and Nunes105
In a subsequent experimental controlled study with community follow-up, a single dose of ketamine infusion (0.71 mg/kg) significantly reduced choices for cocaine cocky-administration versus money, compared with midazolam, among xx cocaine-dependent individuals. Reference Dakwar, Hart, Levin, Nunes and Foltin107 The reduction of cocaine choices in the ketamine group represented a 67% reduction from baseline. Reference Dakwar, Hart, Levin, Nunes and Foltin107 Furthermore, the ketamine group reported significant reductions in cocaine use during the commencement 3 days of follow-up compared with the midazolam grouping, which prodigal at 2 weeks. Reference Dakwar, Hart, Levin, Nunes and Foltin107 A subsequent report from the same sample reported that mystical, only not dissociative, acute effects mediated efficacy. Reference Dakwar, Nunes, Hart, Hu, Foltin and Levin31
A subsequent RCT from the same enquiry group assigned 55 cocaine-dependent patients to either ketamine (0.5 mg/kg) or midazolam (0.025 mg/kg) combined with mindfulness-based relapse prevention therapy. Reference Dakwar, Nunes, Hart, Foltin, Mathew and Carpenter108 At the cease of the 14-day report period, 48% of participants in the ketamine grouping (n = 27) remained abstemious compared with 11% in the midazolam group (n = 28), showing a large effect of ketamine. Reference Dakwar, Nunes, Hart, Foltin, Mathew and Carpenter108 Craving scores were also 58% lower in the ketamine group, and at the 6-month follow-up, 44% of the ketamine group reported cocaine forbearance compared with none of the midazolam group. Reference Dakwar, Nunes, Hart, Foltin, Mathew and Carpenter108
Opioid use disorders
Two RCTs from the one research grouping examined the use of ketamine-assisted psychotherapy for heroin use disorders. Reference Krupitsky, Burakov, Romanova, Dunaevsky, Strassman and Grinenko18,Reference Krupitsky, Burakov, Dunaevsky, Romanova, Slavina and Grinenko19 A trial that compared a higher dose of ketamine (2 mg/kg) to a lower dose (0.2 mg/kg) among 70 detoxified heroin-dependent individuals reported reduced craving in both groups, with a larger effect from the higher dose. Reference Krupitsky, Burakov, Romanova, Dunaevsky, Strassman and Grinenko18 Craving stayed reduced in the loftier-dose group at 24 months, only did not last across 1 month in the low-dose grouping. The rate of abstinence was also higher in the loftier-dose group at both intervals. Reference Krupitsky, Burakov, Romanova, Dunaevsky, Strassman and Grinenko18 A subsequent longitudinal study that compared single versus three sessions of KAP amid 53 heroin-dependent patients reported that participants who received 3 sessions demonstrated a significantly higher abstinence rate of 50% compared with 22% for those who received a single session. Reference Krupitsky, Burakov, Dunaevsky, Romanova, Slavina and Grinenkonineteen
Ketamine may also assist in withdrawal from opiates. The lone RCT in this area reported that ketamine infusion (0.5 mg/kg) was associated with less additional medication required to manage acute opiate withdrawal, but was unrelated to treatment outcome at 4-month follow-up. Reference Jovaiša, Laurinėnas, Vosylius, Šipylaitė, Badaras and Ivaškevičius109
Eating disorders
One open-label trial of ketamine infusion (20 mg/h for 10 h) amidst in-patients with eating disorder diagnoses reported that nine out of fifteen patients showed a marked and sustained return to normal eating behaviour and acceptance of normal weight. Reference Mills, Park, Manara and Merriman110 Variability in follow-up intervals and a somewhat idiosyncratic dosing regimen complicate inferences regarding the duration and generalisability of effects, although these results suggest that further investigation of ketamine therapy for eating disorders is needed.
Adverse effects and risks
2 studies explicitly reported no agin furnishings Reference Krupitsky, Grineko, Berkaliev, Paley, Tetrov and Mushkov16,Reference Krupitsky and Grinenko17 and nineteen did not formally report presence or absenteeism of adverse effects. Reference Kleeblatt, Betzler, Kilarski, Bschor and Köhler48,Reference Papadimitropoulou, Vossen, Karabis, Donatti and Kubitz51,Reference Papakostas, Salloum, Hock, Jha, Murrough and Mathew53,Reference McIntyre, Carvalho, Lui, Majeed, Masand and Gill55,Reference Reinstatler and Youssef61–Reference Witt, Potts, Hubers, Grunebaum, Murrough and Loo66,Reference Rybakowski, Bodnar, Krzywotulski, Chlopocka-Wozniak, Michalak and Rosada-Kurasinska76,Reference Altinay, Karne and Anand84,Reference Shadli, Kawe, Martin, McNaughton, Neehoff and Glue88,Reference Ross, Jain, Bonnett and Wolfson95–Reference Highland, Soumoff, Spinks, Kemezis and Buckenmaier100 The remaining studies all reported adverse effects, with the most common being mild and transient increases in blood pressure level that returned to baseline levels within xxx–120 min. Reference Caddy, Giaroli, White, Shergill and Tracyforty,Reference Wang, Chen, Zhou, Liu, Zhang and Zhang72,Reference Zhang, Rosenheck, Lin, Li, Zhou and Xiao83,Reference Finnegan, Galligan, Ryan, Shanahan, Harkin and Daly87,Reference Shah, McDowell, Ebisu, Hanif and Toerne102,Reference Dakwar, Levin, Foltin, Nunes and Hart106 Tachycardia and bradycardia were besides reported, peculiarly at college doses of ketamine, Reference Fond, Loundou, Rabu, Macgregor, Lançon and Brittnervi,Reference Ray-Griffith, Eads, Han, Golden and Stowe86,Reference Glue, Neehoff, Sabadel, Broughton, Le Nedelec and Shadli89,Reference Taylor, Landeros-Weisenberger, Coughlin, Mulqueen, Johnson and Gabrielninety and more severe cardiac effects. including intermittent atrial fibrillation and single save of ventricular extrasystoles. Were observed in two patients with pre-existing conditions who made a full recovery. Reference Kranaster, Kammerer-Ciernioch, Hoyer and Sartorius70
Most studies too reported transient and dose-dependent dissociative and psychotomimetic effects, including unusual thought content, visual hallucinations and conceptual disorganisation that peaked during and immediately following ketamine infusion and speedily resolved within upwardly to 2 h afterward infusion. Reference Lee, Della Selva, Liu and Himelhochnine,Reference Romeo, Choucha, Fossati and Rotge14,Reference Glue, Medlicott, Harland, Neehoff, Anderson-Fahey and Le Nedelec34,Reference Caddy, Giaroli, White, Shergill and Tracy40,Reference McGirr, Berlim, Bond, Fleck, Yatham and Lam50,Reference Zheng, Cai, Xiang, Zheng, Jiang and Sim52,Reference Rosenblat, Carvalho, Li, Lee, Subramanieapillai and McIntyre54,Reference Fornaro, Carvalho, Fusco, Anastasia, Solmi and Berk58,Reference Zarate, Brutsche, Ibrahim, Franco-Chaves, Diazgranados and Cravchik60,Reference Wang, Chen, Zhou, Liu, Zhang and Zhang72,Reference Dong, Min, Qiu, Chen and Ren85,Reference Finnegan, Galligan, Ryan, Shanahan, Harkin and Daly87,Reference Glue, Neehoff, Sabadel, Broughton, Le Nedelec and Shadli89,Reference Taylor, Landeros-Weisenberger, Coughlin, Mulqueen, Johnson and Gabrielxc Beyond the whole review, in two separate studies, one out of 41 and 31 patients, respectively, discontinued study participation because of dissociative or hallucinatory effects. Reference Okamoto, Nakai, Sakamoto, Nagafusa, Higuchi and Nishikawa71,Reference Feder, Parides, Murrough, Perez, Morgan and Saxena93
Dysphoria and treatment-emergent suicidal ideation were reported in one report. Reference Bloch, Wasylink, Landeros-Weisenberger, Panza, Billingslea and Leckman92 Additionally, there were some reports of transient mania and hypomania that resolved by eighty min following infusion Reference Romeo, Choucha, Fossati and Rotge14 among patients with bipolar disorder who underwent ketamine infusion with Reference Loo, Katalinic, Garfield, Sainsbury, Hadzi-Pavlovic and Mac-Pherson74 or without ECT, Reference Romeo, Choucha, Fossati and Rotgefourteen,Reference Fornaro, Carvalho, Fusco, Anastasia, Solmi and Berk58 although handling-emergent mania was not observed more than frequently in the ketamine group compared with the placebo. Reference Fornaro, Carvalho, Fusco, Anastasia, Solmi and Berk58 Transient increases in anxiety during ketamine infusions are also often reported, with symptoms typically failing within lxxx–120 min, Reference Aan Het Rot, Zarate, Charney and Mathew3,Reference Romeo, Choucha, Fossati and Rotge14,Reference Taylor, Landeros-Weisenberger, Coughlin, Mulqueen, Johnson and Gabrielninety although the review also included two cases of feet persisting upwardly to i–2 days after infusion. Reference Bloch, Wasylink, Landeros-Weisenberger, Panza, Billingslea and Leckman92
Non-dissociative effects associated with ketamine assistants included mild sedation, agitation, nausea and vomiting, headaches, dizziness, blurred vision, dry out or numb mouth, delirium, irritability, sensory changes, urination problems, vertigo and drowsiness; these were overwhelmingly reported to dissipate within one–ii h of ketamine infusion. Reference Aan Het Rot, Zarate, Charney and Mathewthree,Reference Addicted, Loundou, Rabu, Macgregor, Lançon and Brittnerhalf-dozen,Reference Dore, Turnipseed, Dwyer, Turnipseed, Andries and Ascani12,Reference Romeo, Choucha, Fossati and Rotgexiv,Reference Katalinic, Lai, Somogyi, Mitchell, Mucilage and Loo15,Reference Glue, Neehoff, Medlicott, Greyness, Kibby and McNaughton35,Reference Caddy, Giaroli, White, Shergill and Tracy40,Reference Caddy, Amit, McCloud, Rendell, Furukawa and McShane41,Reference Coyle and Laws43,Reference Kishimoto, Chawla, Hagi, Zarate, Kane and Bauer47,Reference Zheng, Cai, Xiang, Zheng, Jiang and Sim52,Reference Fornaro, Carvalho, Fusco, Anastasia, Solmi and Berk58,Reference Run a risk, Bi, Bowen, Weisgerber, Sanjanwala and Prasad69–Reference Wang, Chen, Zhou, Liu, Zhang and Zhang72,Reference Zhong, He, Zhang, Wang, Jiang and Li78,Reference Salehi, Mohammadbeigi, Kamali, Taheri-Nejad and Moshiri82,Reference Zhang, Rosenheck, Lin, Li, Zhou and Xiao83,Reference Dong, Min, Qiu, Chen and Ren85,Reference Finnegan, Galligan, Ryan, Shanahan, Harkin and Daly87,Reference Glue, Neehoff, Sabadel, Broughton, Le Nedelec and Shadli89–Reference Rodriguez, Kegeles, Levinson, Feng, Marcus and Vermes91,Reference Feder, Parides, Murrough, Perez, Morgan and Saxena93,Reference Wong, Benedict, Armahizer and Kane-Gill101,Reference Pizon, Lynch, Benedict, Yanta, Frisch and Menke103,Reference Dakwar, Levin, Hart, Basaraba, Choi and Pavlicova104,Reference Dakwar, Nunes, Hart, Foltin, Mathew and Carpenter108,Reference Mills, Park, Manara and Merriman110
We found no reports of ketamine use/misuse following treatment with ketamine, nor is in that location testify of transition from medical to non-medical ketamine utilise. Reference Dore, Turnipseed, Dwyer, Turnipseed, Andries and Ascani12,Reference Rosenblat, Carvalho, Li, Lee, Subramanieapillai and McIntyre54
Risk of bias
The results of the risk-of-bias analysis is reported in Supplementary Appendix 1 for randomised studies, Supplementary Appendix 2 for non-randomised studies and Supplementary Appendix 3 for systematic reviews/meta-analyses. Most randomised trials were judged to be at either loftier risk of bias or raise some concerns in at to the lowest degree ane domain. Most common areas of concern were option of the reported results, randomisation and allocation concealment, deviations from intended interventions, missing data and measurement of effect. Most non-randomised studies were also judged to be at serious adventure of bias. All non-randomised studies suffered from take a chance of bias considering of a lack of command and measurement for baseline confounding, and all except i was judged to be at serious risk of bias because of the measurement of outcome. Other areas of concern included retrospective classification of outcomes, selection bias, deviations from intended interventions and missing effect data. According to the AMSTAR Checklist, the majority of the systematic reviews were of critically low quality. Frequent critical bug were lack of reference to a registered review protocol, and lack of hazard-of-bias analysis and consideration of risk of bias in the interpretation of findings.
Discussion
Involvement in ketamine therapies for mental wellness concerns expanded dramatically between 2010 and 2020 (Fig. 2). Contempo FDA and European Medicines Agency approvals for esketamine in treatment-resistant depression and the broader re-emergence of psychedelic medicines prognosticate accelerating utilise and demand for ketamine in mental wellness treatment over the coming decade. The current review focused on the areas nosotros feel are most central to clinical practice: affective disorders, suicidal ideation, anxiety disorders, post-traumatic stress disorder, obsessive–compulsive disorder, substance use disorders and eating disorders.
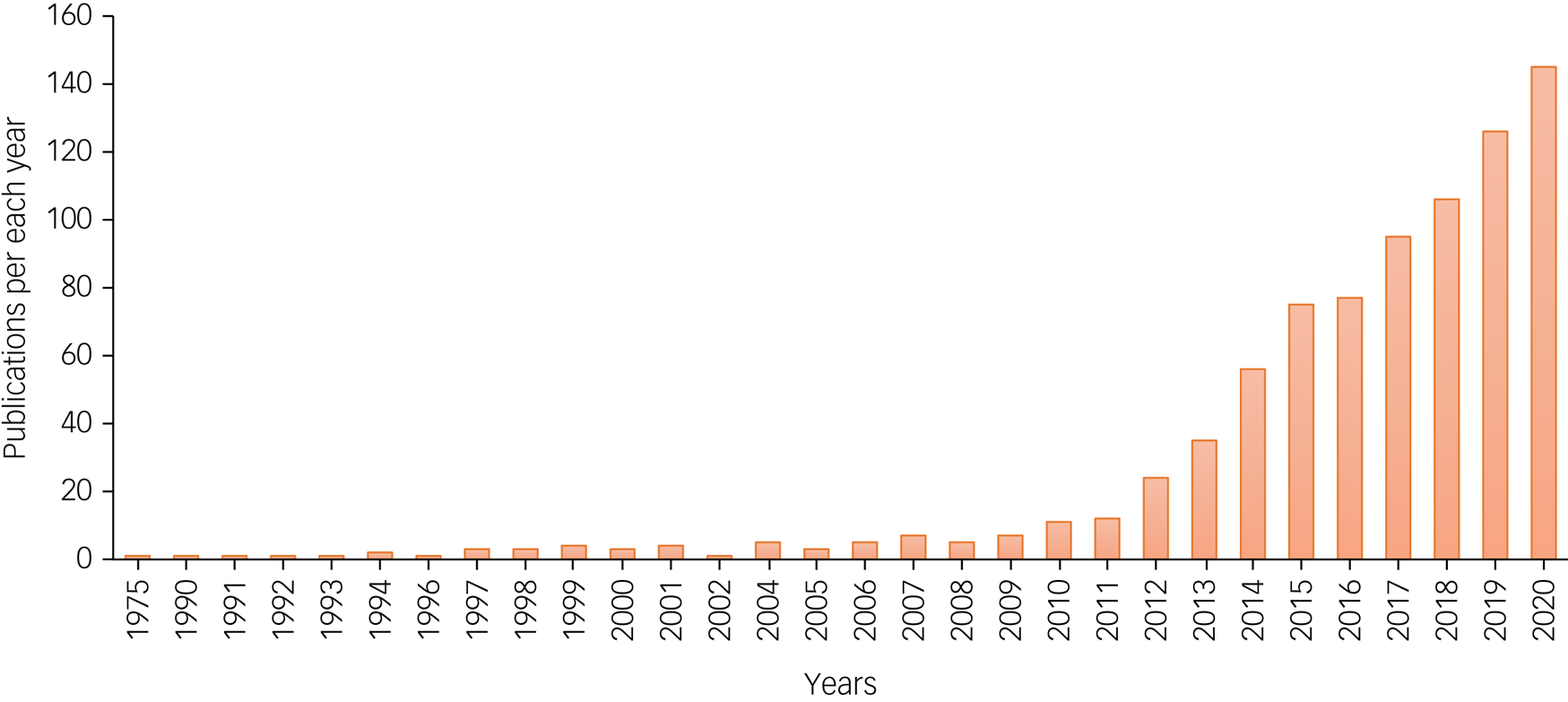
Fig. 2 Number of publications with search terms ketamine and mental health in PubMed per year, from 1975 till Dec 2020.
Affective disorders and suicidal ideation are the category of psychopathology with the most robust show regarding ketamine therapies, based on multiple systematic reviews and meta-analyses. Although there was some show to support effectiveness of ketamine assistants for other indications (post-traumatic stress disorder, obsessive–compulsive disorder, anxiety and substance apply disorders), the bear witness base comprised a modest number of mostly non-randomised trials with ofttimes short follow-up periods, therefore requiring corroboration and extension. The challenges to estimation presented by this paucity of testify are exacerbated by cross-study variations in dose, modes of administration and adjunctive therapies, the combination of which complicates the determination of what works for whom. Enquiry to optimise adjunctive psychotherapy and the broader 'set and setting' of ketamine experiences are besides required to estimate the parameters of ketamine effects in the context of psychological health. Nonetheless, extant evidence provides signals that permit some conditional observations.
Beyond all studies where handling effects accept been consistently observed, there is a need to profile treatment responders, along with identifying dose and route of administration and other factors that may prolong the effectiveness of ketamine therapy. Additionally, further inquiry with comparisons to agile placebos is required to evaluate comparative efficacy. Attempts to calculate the comparative efficacy of dissimilar administration routes are burdened by the heterogeneity across studies, particularly with regards to frequency of assistants: studies examining intranasal ketamine involve repeated doses, whereas most studies on intravenous ketamine consist of a single infusion. Reference McIntyre, Carvalho, Lui, Majeed, Masand and Gill55 Enquiry that explores means of extending effect duration is likewise required to place best practices for ketamine in the context of psychiatric disorders. In add-on to specifying optimal duration and frequency of dose, determining the extent to which clinical training, integration and guidance during the acute feel extends the elapsing and power of therapeutic furnishings is a research priority, as is the further elucidation of the importance of subjective effects such as mystical experiences.
From a more practical standpoint, evaluating modes of administration such equally intramuscular and intranasal, which are less invasive and demanding of clinical resources, may exist important for reducing barriers to access. The brunt of affective disorders is borne unduly by those at lower levels of socioeconomic condition, Reference Freeman, Tyrovolas, Koyanagi, Chatterji, Leonardi and Ayuso-Mateos111 and as such, research should also focus on ways of ensuring accessibility and equity in the delivery of ketamine therapies, including testing racemic ketamine against enantiomers. Finally, extant research does not speak conclusively to the rubber of repeated administration over fourth dimension, and as such, longitudinal enquiry on safety is essential for informed estimation of risks and benefits of ketamine relative to other therapeutic options.
The combined anaesthetic and antidepressant effects of ketamine make information technology an appealing adjunct during ECT for depression, and our review suggests that the addition of ketamine to ECT tin lead to longer seizure elapsing, fewer required treatment sessions, accelerate symptom reduction and fourth dimension to remission. The therapeutic furnishings of ketamine with ECT take been most comprehensively demonstrated for treatment-resistant depression, Reference Kranaster, Kammerer-Ciernioch, Hoyer and Sartoriuslxx,Reference Okamoto, Nakai, Sakamoto, Nagafusa, Higuchi and Nishikawa71,Reference Salehi, Mohammadbeigi, Kamali, Taheri-Nejad and Moshiri82 with less robust adjunctive effects in MDD and bipolar disorder, highlighting the need for further inquiry to analyze when and for whom ketamine might accentuate the benefits of ECT.
Given that ketamine may besides be used recreationally, information technology is notable that even in addiction treatment, no studies in our review report a transition to illicit use engendered by introduction to ketamine in a therapeutic context. Future inquiry should continue to monitor this potential adverse effect of ketamine therapy in the context of substance use disorders. However, given the negative consequences of substance use disorders, peculiarly the grave harm of overdose associated with opioid misuse, the relatively small risks of ketamine misuse should not present a bulwark to treatment for opioid use disorders or for psychiatric comorbidities that may accompany opioid misuse. Conversely, patients who apply ketamine outside of medical supervision should be queried to determine the extent to which this utilize might reflect therapeutic motives as a drug substitute or to accost negative affect.
Several areas warrant farther research. In particular, the importance of subjective experience and adjunctive psychotherapy in relation to the effects of ketamine are key areas where the extant literature is limited past the lack of more rigorous randomised control designs, which have been effective in bolstering the bear witness for other forms of psychedelic-assisted psychotherapy such as MDMA-assisted psychotherapy Reference Mithoefer, Feduccia, Jerome, Wagner, Walsh and Hamilton112 and psilocybin-assisted psychotherapy. Reference Carhart-Harris, Bolstridge, 24-hour interval, Rucker, Watts and Erritzoe113 Farther research should too try to elucidate the mechanisms by which ketamine furnishings such a wide range of mental health conditions. The apparent diversity of ketamine therapeutic action has led to speculation regarding potential cross-cut mechanisms, including the proposal that ketamine may bear upon the college-order personality trait of neuroticism, Reference McNaughton and Mucilage114 enhance mindfulness and provide therapeutic experiences of self-credence and absence of negative emotions, Reference Dore, Turnipseed, Dwyer, Turnipseed, Andries and Ascani12 just these interesting proposals have not been subject to rigorous tests.
In that location is also surprising paucity of research on ketamine treatment for personality disorders and eating disorders. We identified no reports on personality disorders and 1 small open-label trial for eating disorders. In light of recent involvement in the use of psychedelic-assisted psychotherapy for eating disorders and the limited treatment options for eating disorders, farther examination of the therapeutic potential of ketamine for eating disorders is warranted. Reference Hermens, Simcock, Dutton, Bouças, Can and Lilley115–Reference Keeler, Patsalos, Thuret, Ehrlich, Tchanturia and Himmerich118 With regard to personality disorders, the loftier levels suicidality associated with deadline personality makes research on ketamine for suicidality also a priority among this population. Moreover, in light of the positive effects of ketamine for depressive disorders, the lack of research on the utilize of ketamine in the treatment of postpartum depression is a notable gap that demands consideration.
The most common adverse effects associated with ketamine administration were increases in systolic and diastolic blood pressure level, dissociation and psychotomimetic symptoms, all of which were brusk lived. Withal, given the relatively nascent state of research and do in the surface area of ketamine for mental wellness, further research is required to definitively decide the condom and tolerability of ketamine in psychiatric populations, specially over the longer term. Nonetheless, extant show on the risks of ketamine advise a profile that is comparable to other widely used psychiatric medications.
The electric current review provides a comprehensive overview of the evidence base of operations for ketamine treatment across psychiatric disorders, including depression, bipolar disorder, anxiety disorders, mail service-traumatic stress disorders, obsessive–compulsive disorders, substance use disorders and eating disorders. We used an extensive search strategy roofing a number of databases and trial registries to identify all relevant literature. All the same, there are a number of limitations to consider. Outset, considering of the high number of studies included in the review, single review authors undertook data extraction and rated risk of bias; even so, all reviewers were trained in using the forms, and a selection of data extraction and risk of bias forms were piloted for accurateness and abyss. It is as well worth noting that bulk of the studies included in the review were rated as at high risk of bias because of a number of methodological limitations outlined in the risk of bias results, and then the results should be interpreted with caution. Moreover, although testify from MDD suggests that ketamine furnishings and risks are consequent across use of concomitant medications, further research is required to assess the extent to which these plainly robust furnishings generalise to other conditions and beyond diverse classes of medications. In particular, it may be interesting to examine the extent to which ketamine effects collaborate with those of other interventions emerging under the banner of psychedelic-assisted psychotherapy. Additionally, included studies were heterogenous in terms of ketamine administration (dose, number, route of delivery), measurement of outcomes, length of follow-upward, study blueprint and setting, which reduces comparability.
There are a number of methodological differences between ketamine studies that would benefit from standardising to aid interpretation of findings as more psychiatric indications are researched as targets for ketamine handling. One area of discrepancy has been the use of active (typically midazolam) versus inactive placebos (typically saline). Although earlier studies in depression used inactive placebos, active placebos have begun to be adopted. Benefits of active placebos are in providing more confidence in blinding to handling allocation, where the subjective furnishings of the drug make blinding hard, every bit with ketamine. Concerns virtually active placebos are that they may accept unintended treatment consequences; for instance, in studies for anxiety, where benzodiazepines are used every bit a treatment. However, in the studies reviewed here, this is not consistently observed; for instance, in the written report by Dakwar et al, Reference Dakwar, Levin, Hart, Basaraba, Choi and Pavlicova104 more than individuals dropped out from the midazolam group and returned to heavy drinking compared with the ketamine grouping. Amid those with feet disorders, midazolam had small transient effects on anxiety symptoms, equivalent to 0.25 mg/kg ketamine, Reference Glue, Neehoff, Sabadel, Broughton, Le Nedelec and Shadli89 suggesting that using midazolam as agile control at higher doses of ketamine (e.g. 0.five mg/kg) should not obscure the active treatment event. In addition to using active placebos, some researchers take attempted to minimise expectancy effects by informing the participants that they may receive any one of a number of psychoactive drugs, including ketamine. Reference Dakwar, Levin, Hart, Basaraba, Choi and Pavlicova104,Reference Dakwar, Anerella, Hart, Levin, Mathew and Nunes105 Futurity trials of ketamine or other drugs with identifiable psychoactive furnishings can too minimise bias by having independent effect assessors who are non present during drug administration.
Similar differences have been in the use of cross-over studies (within participants) or betwixt-participant designs. The merit of the old is the ability to observe effects in the same participants, thus negating the consequence of pre-existing group difference, only it can exist confounded past persisting handling and social club effects. Similarly, with studies where participants all have function in both arms, this can compound blinding bug fifty-fifty where participants are given active placebos. Upon reviewing the literature, nosotros would recommend the use of active placebos where possible, in between-participant designs.
Numerous avenues are ripe for exploration in future treatment approaches with ketamine. One area of interest is in creating trials to tackle the trouble of comorbidities and multi-morbidities, which are ofttimes more than representative of the psychiatric population at large, where 'pure' diagnoses are rare. Ketamine seems a good solution to the trouble of multi-morbidities every bit it is emerging every bit an effective treatment for a number of atmospheric condition, and this raises the issue of whether strict diagnostic criteria that have been used in the by should be considered for entry into clinical trials, or whether expanding to treat presenting symptoms with a conception-based approach may be more appropriate.
Trials accept likewise only begun to investigate the synergies between ketamine and psychological therapy, and future research should design full factorial approaches to assess both the additive and interactive effects of combining such interventions. Based on the extant literature, it is difficult to prescribe fifty-fifty a minimum adequate behavioural framework for giving ketamine clinically, but research from clinical apply of KAP Reference Dore, Turnipseed, Dwyer, Turnipseed, Andries and Ascani12 and qualitative studies in the field Reference Mollaahmetoglu, Keeler, Ashbullby, Ketzitzidou-Argyri, Grabski and Morgan119 suggest that sufficient preparation before the experience, a clinical and professional person setting and trusting and supportive relationships with staff is crucial, every bit patients are very sensitive to small disruptions in the setting. Given findings that ketamine's therapeutic benefits can be extended with psychological therapy, Reference Wilkinson, Wright, Fasula, Fenton, Griepp and Ostroff29,Reference Rodriguez, Wheaton, Zwerling, Steinman, Sonnenfeld and Galfalvy120 information technology is advisable to provide ketamine handling aslope a psychological therapy. Sure psychological therapies may be particularly compatible with ketamine treatment. For example, combining ketamine with motivational enhancement therapy may further increase motivation to remain abstemious in alcohol and substance use disorders, because of ketamine'southward effect on increasing motivation to quit drug use. Reference Dakwar, Levin, Foltin, Nunes and Hart106 Alternatively, because of ketamine's mystical and spiritual effects, it may serve to deepen the mindfulness exercise cultivated by mindfulness-based therapies. However, selection of adjunctive therapy should also be informed by the symptoms of the patient population.
Another important consideration in trial pattern is representativeness of the trial population and access to these trials, and later therapies by individuals from disadvantaged groups. Inequalities in access to healthcare are replicated in admission to clinical trials, with some exceptions. Reference Dakwar, Levin, Foltin, Nunes and Hart106–Reference Dakwar, Nunes, Hart, Foltin, Mathew and Carpenter108 Trials neglect to consistently written report on ethnicity and socioeconomic status, which are important to approximate the generalisability of the findings to the population at big, and should exist considered a minimum standard of clinical trial reporting. Recent efforts in this inquiry infinite to create culturally informed research designs (e.g. Williams et al Reference Williams, Reed and Aggarwal121) should be translated to ketamine research and are of import examples of ways to diversify enquiry in this field, an area that has been hitherto neglected and is urgently needed. Reference Williams and Labate122
In determination, the plethora of prove from the systematic reviews and meta-analyses reviewed here supports a robust, rapid and transient antidepressant effect of ketamine in unipolar and bipolar depression, equally well as treatment-resistant depression, with repeated dosing increasing the duration of effectiveness. In numerous studies, ketamine was likewise demonstrated to accept short-lived anti-suicidal properties, independently of improvements in depressive symptoms. A pocket-sized number of trials provide some evidence to support the beneficial furnishings of ketamine for post-traumatic stress disorder and obsessive–compulsive disorder. Ketamine's anxiolytic effects for social anxiety disorder and generalised anxiety disorder have likewise been reported, nonetheless symptom recurrence following treatment was common. There is likewise evidence that ketamine results in brusk-term increases in abstinence, reductions in use, cravings and symptoms of withdrawal related to problematic substance use. In lite of the substantial mortality associated with opioid overdose, the potential of ketamine to address opioid use disorders is specially encouraging and worthy of farther investigation.
Notably, the majority of the research we reviewed was classified as being at high adventure of bias, as nigh studies are small and have other methodological limitations. There is also much still to make up one's mind regarding synergistic furnishings with psychological therapy and to better specify therapeutic modalities. Research on optimal dose, road and frequency of administration that foregrounds accessibility and equity will also be paramount to reduce barriers to admission amongst the lower income and marginalised communities that are disproportionately affected by the weather condition for which this promising handling may be effective. In sum, despite of import unknowns regarding ways of prolonging effects and risk over time associated with long-term repeated use, interest in the psychiatric applications of ketamine has accelerated dramatically over the by decade. This interested is warranted given ketamine's broad spectrum of potential applications in psychiatric treatment, with limited adverse furnishings. In lite of recent progress in the development and application of ketamine-based psychiatric medicines, likewise equally broader developments in psychedelic-assisted psychotherapy, it seems well-nigh certain that interest and uptake of psychiatric utilise of ketamine will expand fifty-fifty further in the decades to come up.
Source: https://www.cambridge.org/core/journals/bjpsych-open/article/ketamine-for-the-treatment-of-mental-health-and-substance-use-disorders-comprehensive-systematic-review/36E261BFA62CDA6459B88F7777415FDA
0 Response to "Psychedelics in the Treatment of Unipolar Mood Disorders a Systematic Review"
Enregistrer un commentaire